That’s the so-called liposoluble vitamin, which, like other vitamins and minerals, belongs to the group of micronutrients that must be ingested in the body, but in minimal quantities – our body has no possibility of their endogenous synthesis.
Since 1929, the Danish scholar Henrik Dam and Edward Adelbert Doisy from the University of St. Lewis, working in parallel until 1939, discovers a molecule that is positioned in the category of vitamins and initially gets the letter K, after publishing their work in a German scientific journal and is called “Coagulation vitamin”. These two scientists receive the Nobel Prize in Medicine in 1943 for their discovery. But until 1974, the precise function of vitamin K was not known, that is till the discovery of prothrombin, a vitamin K dependent coagulation factor in three independent laboratories by Stenflo, Nelsestuen and Magnusson.
Today’s findings point to the following significant functions of vitamin K functions in body homeostasis:
- Blood coagulation: It takes part in the production of prothrombin (factor II), the coagulation factors VII, IX, and X, as well as the proteins C, S and Z
- Participate in bone metabolism through osteocalcin known as “bone Gla protein”, Matrix Gla protein, periosthenes and recently discovered Gla-rich protein.
- Normal functioning of blood vessels through the so-called Gas6 protein plays a significant role in cell proliferation, but also plays a role in the hormone by stimulating beta cells in the pancreas to release more insulin, while simultaneously stimulating fat cells to release the hormone adiponectin that increases the insulin sensitivity.
- The role of recently detected proline-rich γ-carboxyglutamyl prenoins (PRGPs) 1 and 2, and transmembrane γ-carboxy glutamyl proteins (TMGs) 3 and 4 are still not sufficiently known.
It is known that the activity of “vitamin K-dependent” coagulation factors in the neonatal period reaches a maximum of 60% of the normal values in adults. This is due primarily to small vitamin K stores in infants and infants due to small fetal stocks due to the fact that vitamin K in minimal amounts passes through the placenta. On the other hand, there is a delayed synthesis of vitamin K in the intestine, as well as significantly lower vitamin K concentrations in human milk compared to milk formulas.
In human milk in 100 ml there is 0.1-0.2 ug of vitamin K, while in milk formulas for children it ranges from 5-20 micrograms. If we take into account the daily needs that reach 25 μg, the so-called “physiological hypoprothrombinemia” in newborns and children in the first three months of life in babies who are breast-feeding.
Sometimes the above-mentioned hypoprothrombinemia reaches a degree when it is not possible to maintain spontaneous haemostasis and there is a haemorrhagic neonatal disease. This clinical condition is immensely significant because of its morbidity, mortality and consequences.
It can occur extremely rarely as early haemorrhagic disease of the newborn during the first day of life, most often in mothers receiving anti-epileptics and is transmitted by severe and lethal bleeding in the central nervous system.
It can occur as a classical haemorrhagic neonatal disease between 2-7 days of life and in 0.25-1.7 newborns at 100 births. Clinical bleeds are most often not life threatening and can occur in the gastrointestinal system, papilloma, or at the injection site in a newborn child.
A third form is late haemorrhagic neonates that occur in 2-10 newborns at 100,000 births. In just over 70% of cases, there are heavy corpora in the central nervous system with high mortality, which reaches 50%.
The high incidence of classical form and the severe clinical picture of late hemorrhagic disease of the newborn are the main reasons for prophylactic use of vitamin K1 in all newborns. The prophylactic use of vitamin K was initiated in the United States in the 1960s when the American Academy of Pediatrics recommended the parenteral injection of vitamin K1 as a prophylaxis of hemorrhagic disease of the newborn. This approach with the application of 1 mg of vitamin K parenterally for infants and 0.5 mg for preterm babies is accepted by most countries in the world, including in our country.
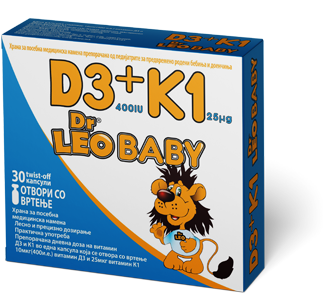
It is apparent that despite a one-time application of vitamin K, there may be a low activity of vitamin K-dependent coagulation factors and develop late hemorrhagic disease of the newborn in a large number of countries, supplemental supplementation with 25 ug vitamin K has been introduced. Such prolonged oral prophylaxis has been introduced by European countries such as the UK, the Netherlands, Poland, Italy, France, Serbia, but also in our country. In Canada, New Zealand and Australia, oral prophylaxis has been introduced in those children whose parents refuse intramuscular application.
This recommendation is initially at the birthplace of intramuscular application of vitamin K1 immediately after birth at a dose of 1 mg for infant newborns and 0.5 mg for premature babies. Then continue prophylaxis from the 7th day to the end of the third month of life by inserting 25g of vitamin K1 daily in children who are breast-feeding. In children who are on an artificial diet it is not necessary because in the formulas is added vitamin K. Prolonged oral prophylaxis is of great significance for premature babies, infants and infants with severe and prolonged jaundice, but also in those where antibiotic and antipyeleptic therapy is used both in the child and in the mother.